Two refugees and a foreign student on a visa brought multi-drug resistant (MDR) tuberculosis (TB) to Milwaukee, Wisconsin in 2009 and 2011, according to a 2014 article in an epidemiology publication written with the cooperation of the doctors who treated them.
The introduction of MDR TB to the United States represents a serious public health threat, since its successful treatment is uncertain and very expensive. Active TB can usually be treated successfully in six to nine months at a cost of $17,000 per patient, according to the Centers for Disease Control (CDC), but MDR TB treatment costs more than $150,000 per patient and can take between 20 and 26 months.
The six to nine month treatment regimen for active TB, which has been standard practice in the United States for some 50 years, involves a combination of four drugs: rifampin, isoniazid, pyrazinamide, and ethambutol.
Over the past several decades, new strains of TB have developed around the world which are resistant to at least two of these four drugs, hence the term MDR TB. Treatment for MDR TB begins only after the patient is observed to be resistant to the standard four drug protocol. Subsequent to diagnosis, a number of expensive “second level” drugs are added to the patient’s treatment regimen.
Twenty cases of MDR TB, all foreign-born, were diagnosed in Wisconsin over the eight year period between 2005 and 2012, according to the Wisconsin Department of Health Services.
Twelve of these cases were from the Hmong people in Laos (though Case 2 in the 2014 article was categorized as “drug resistant,” not formally MDR-TB, it was probably included among these 12, as well as Case 2’s “close household contact”), four were from India (including Case 3 from the 2014 article), one was from Burma (including Case 1 from the 2014 article), and one each were from China, Ethiopia, and Nepal.
State and local taxpayers in Wisconsin paid for the treatment of these twenty foreign-born cases of MDR TB. At a cost of $150,000 per patient, the total cost was an estimated $3 million.
“Over 70,000 refugees and former refugees live in Wisconsin. Of this number, the great majority (about 55,000) are Hmong from Laos in Southeast Asia, but refugees have come to Wisconsin from all over the world. . . The newest come from Somalia, former Burma (Karen and Chin) and Bhutan (next to Nepal, China and India),” the Wisconsin Department of Children and Families reports.
Unlike fourteen other states, Wisconsin has not withdrawn from the federal refugee resettlement program. Luther Social Services of Wisconsin is the leading voluntary agency (VOLAG) that resettles refugees in the Milwaukee area based on a contractual relationship with the federal government and with the cooperation of the state government.
Case 1 in the 2014 article was a “21-year-old Burmese woman [who] entered the USA in April 2009 after staying in a refugee camp in Thailand.”
It is not clear whether this 21-year-old Burmese woman underwent the overseas medical screening required of refugees seeking to be settled in the United States under the program supervised by the federal Office of Refugee Resettlement and designed by the Centers for Disease Control (CDC), which is supposed to identify “high risk” tuberculosis cases prior to entry.
In any event, upon arrival in the United States, both the 21-year-old Burmese woman and her father were diagnosed with active TB, the article indidates.
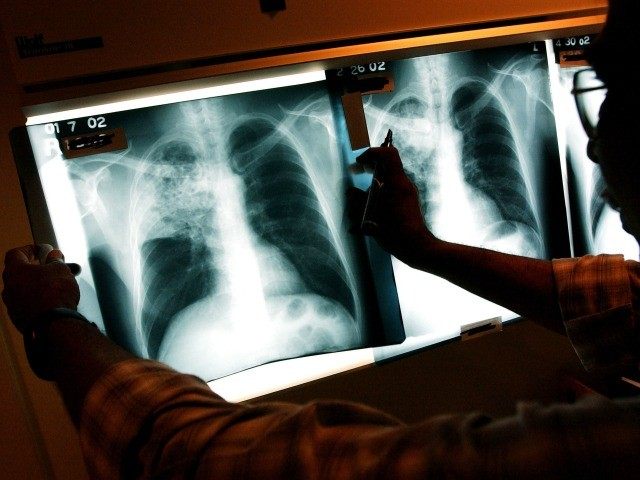
“Her father was treated for pan-sensitive active tuberculosis (TB), and her mother and two siblings had latent TB infection. The patient was considered an active case based upon a preliminary investigation (smear-negative but chest X-ray abnormal, [latent TB infection] test-positive),” the authors note.
Her case of active TB quickly became MDR TB.
Case 2 in the 2014 article was a “22-year-old Hmong woman [who] entered the USA in September 2009 after staying at a different refugee camp than case 1 in Thailand. Initial chest X-ray, sputum, and [latent TB infection] tests were negative.”
Based on this description, this 22-year-old Hmong woman was probably not flagged at all in her overseas medical screening and allowed to enter the United States under the refugee resettlement program.
But more than a year after arriving in the United States, she developed active TB, which quickly turned into drug-resistant TB. The authors of the study suggest the case should probably have been classified as MDR TB.
“In August 2011, the patient was negative by smear microscopy but exhibited an abnormal chest X-ray and was treated at TBCC [the City of Milwaukee Health Department’s Tuberculosis Control Clinic of the Keenan Health Center]. . . [T]he patient was a close household contact of a person with isoniazid-resistant, pulmonary TB,” the authors of the 2014 article write.
Case 3 in the 2014 article was a “32-year-old woman from India [who] entered the USA in May 2011 on a student visa. The patient presented with a prior history of TB (pan-sensitive in 2009), and developed high fever and cough 6 months after entering the USA. She was treated at TBCC where a preliminary evaluation revealed smear-positive sputum and an abnormal chest X-ray with cavitary lung lesions,” indicating she had active infectious TB.
Worldwide, the number of MDR TB cases has increased from 273,000 new cases in 2000 to 480,000 new cases in 2014. During that same time, the number of new active TB cases worldwide each year has fluctuated around 9 million.
In 2014, an estimated 1.5 million people (17 percent of the new TB cases that year) died of TB. Of those, 190,000 died of MDR TB (39 percent of the new MDR TB cases that year). In the United States, 550 people died of the 9,421 new cases that year (one half of 1 percent). (Note: the overall number of active TB cases increased by 1.7 percent in 2015 to 9,563).
There were 91 reported cases of MDR TB in the United States in 2014, but CDC has not provided data on the number of MDR TB deaths that year.
The higher worldwide morbidity rate of TB, compared to the United States, is largely due to the fact that almost every new patient in our country goes through the six to nine month regimen with the standard treatment of those four usually reliable drugs: rifampin, isoniazid, pyrazinamide, and ethambutol.
Many TB patients in other parts of the world never receive this standardized treatment, even though it has been a standard protocol in the United States since the 1950s.
The higher morbidity rate of MDR TB compared to active TB (39 percent vs. 17 percent) is an indication that a number of patients with this version of TB never receive the more expensive recommended treatment, and that the treatment itself is not always successful.
MDR TB has historically been less of a threat in the United States, but that may be changing.
In 1993, there were only 486 cases of MDR TB reported here. That number had dropped to 91 cases in 2014.
The demographics of MDR TB within the United States, however, has changed dramatically over these two decades.
In 1993, only 25 percent of the 486 MDR TB cases were foreign born. By 2014 that number had skyrocketed to 90 percent of the 96 cases reported in 2013.
But there’s even more troubling TB health news on the horizon.
“Extensively Drug-resistant TB (XDR TB) is a rare type of MDR TB that is resistant to isoniazid and rifampin, plus any fluoroquinolone and at least one of three injectable second-line drugs (i.e., amikacin, kanamycin, or capreomycin),” the CDC reports.
“Because XDR TB is resistant to the most potent TB drugs, patients are left with treatment options that are much less effective,” the CDC notes.
The CDC estimates that XDR TB can take 36 months to treat at a cost of $482,000 per patient, more than triple the cost of treating MDR TB, and more than 25 times the cost of treating a patient with active TB.
“A total of 83 cases of XDR-TB were reported in the United States from 1993 to 2007,” one recent report notes, adding, “Worldwide emergence of extensively drug-resistant tuberculosis (XDR-TB) has raised global public health concern, given the limited therapy options and high mortality.”
There was at least one case of XDR TB in the United States in 2015, a traveler from India, as NBC reported.
Current immigration trends in the United States, in which most new foreign-born residents come from Asia, Africa, the Middle East, South America, and Central America, suggest that MDR TB and XDR TB may become an increasing public health threat in the United States.
“Increasing cases of multidrug-resistant (MDR) and extensively drug-resistant (XDR) strains of Mycobacterium tuberculosis … continue to emerge, particularly from Asia and Africa, the 2014 article on migrants bringing MDR TB to Wisconsin notes.
“Drug-resistant TB is emerging in many parts of the world; however, characterization of these strains remains incomplete. ..Use of inappropriate or intermittent TB therapeutic measures may lead to the emergence of new resistant strains and challenge effective therapy,” the 2014 article adds.
The authors of the article close by sounding the alarm bells for the United States.
“Political unrest, war, poverty, and famine will continue to lead to migration of refugees and immigrants from TB-endemic areas into the USA,” the authors observe.
“The next resistant TB strain may be just one plane journey away,” they conclude.
COMMENTS
Please let us know if you're having issues with commenting.