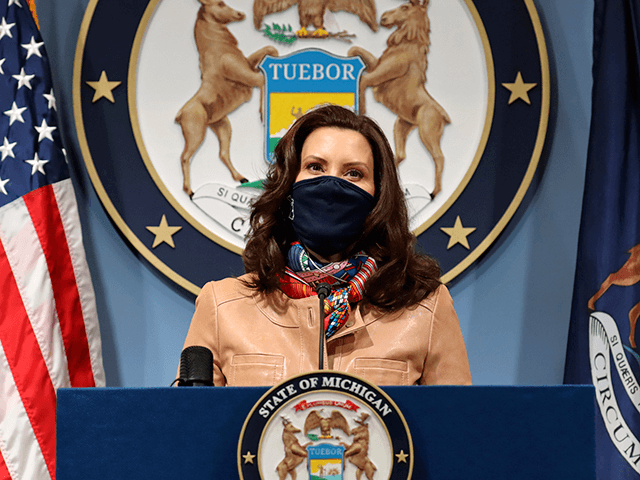
Michigan Gov. Gretchen Whitmer faces her latest coronavirus-related challenge as her state is currently unable to meet the demand of patients seeking monoclonal antibody treatments, according to a report from the Detroit Free Press.
The state does not have enough doses of monoclonal antibodies to meet demand and lacks an adequate number of health care workers to administer them, health experts told the outlet.
Department of Health and Human Services Spokesperson Lynn Sutfin told the Detroit Free Press: “Based on the amount of medication being allocated to Michigan by the federal government, as well as the amount of medication being used throughout the state, there is not enough supply at this time.”
In November, Spectrum Health in Grand Rapids received up to 1,000 calls daily when demand for monoclonal antibodies was peaking, but the hospital could only administer 400-450 treatments weekly, the outlet reports.
“That’s a pretty significant mismatch,” said President of Spectrum Health West Michigan Dr. Darryl Elmouchi. Spectrum Health West Michigan hopes to increase the number of infusions to 500 a week.
“There’s two limiting variables for monoclonal antibodies. No. 1 is the supply of monoclonal antibodies, which for the most part has been our biggest limitation,” Elmouchi said. “But No. 2 is to have enough staff to be able to administer it because it is labor intensive.”
“You need health care providers who can do infusions… Staffing, it’s hard. It’s a hard job and you’ve got to find people who are qualified to do it,” he added.
The monoclonal antibody treatment process takes roughly an hour and a half per patient, and nurses usually administer the therapy, but nurses and staff are stretched thin.
Citing the latest state data, the Detroit Free Press reports that eight of the state’s hospitals were at full capacity on Friday, while an additional thirty hospitals reported 90 percent occupancy.
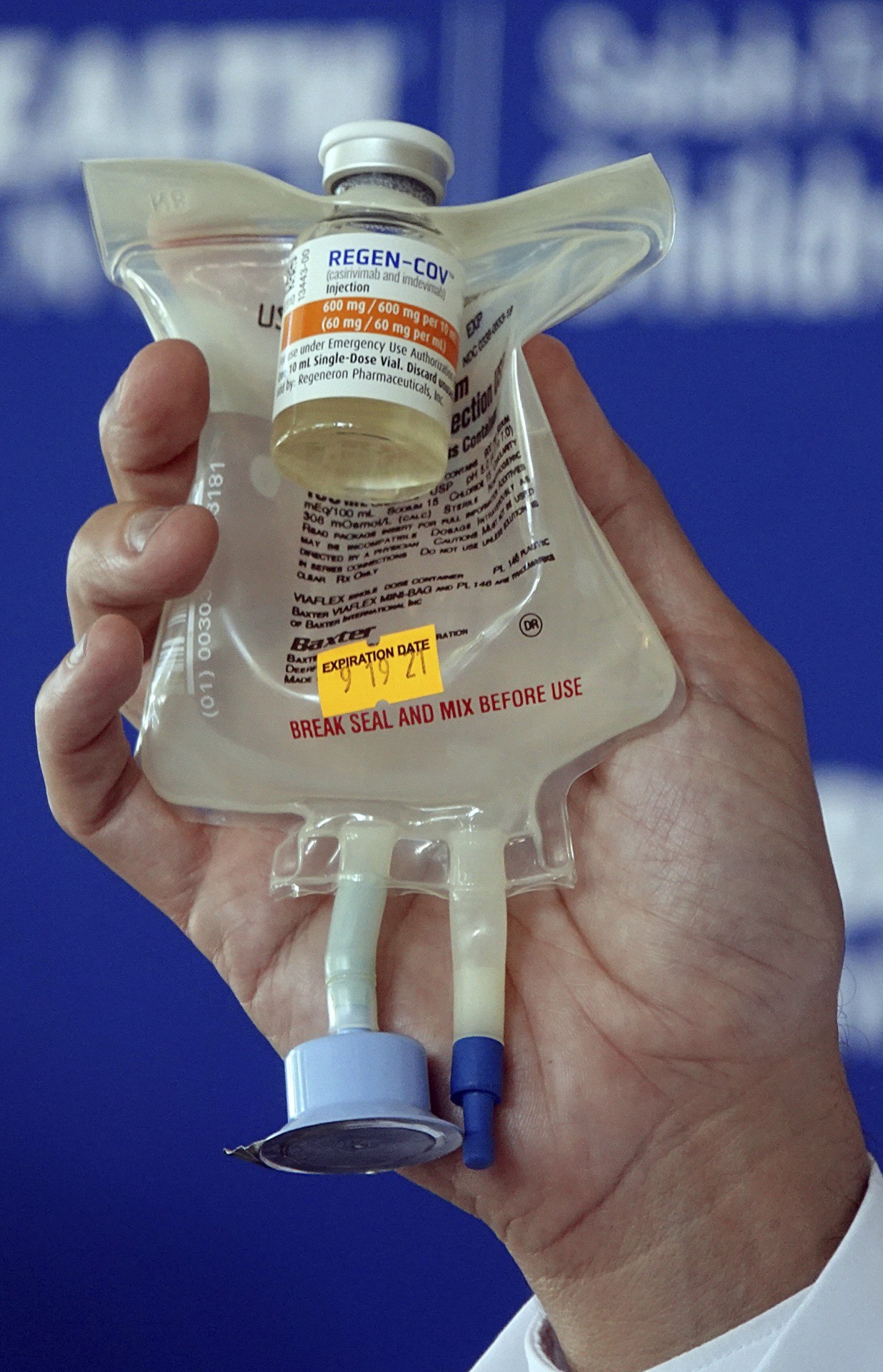
Dr. Aldo Calvo, Medical Director of Family Medicine at Broward Health, shows a Regeneron monoclonal antibody infusion bag during a news conference Thursday, Aug. 19, 2021 at the Hospital in Fort Lauderdale, Fla. (Joe Cavaretta/South Florida Sun-Sentinel via AP)
“We’re redirecting all of our staff to our hospitals, and we have shut down clinics and surgeries and so many things,” Elmouchi said. “That’s our first priority because we have to take care of the sickest people first, but we want to keep this going as best we can.”
President and CEO Dr. Bruce Muma of the Henry Ford Health System Physician Network struggles through similar setbacks as Elmouchi. In the last week, Henry Ford received roughly 2,000 requests for monoclonal antibody therapy but could only doll out 725 treatments.
Muma told the Detroit Free Press, “By hook or by crook, we’re expanding our capacity every week.”
Muma stated:
One of our infusion centers expanded their hours to 3:30 in the morning … because there was a subset of ER nurses who were so concerned about what they were seeing in the ER that they wanted to start doing something to prevent patients from needing to be in the hospital. So they are … coming in four hours early for this shift.
Other hospitals are undergoing a similar squeeze. Beaumont Health network in southeast Michigan currently has a waiting list for treatments as the hospital system receives 600-700 requests weekly, said spokesman Mark Geary. The health system is only able to administer 145 treatments a week, he noted.
Michigan Medicine receives 380 therapy requests weekly but can only provide 150 doses in a week’s time, according to the Detroit Free Press.
“We are limited by workforce shortages and are prioritizing patients who are at highest risk for hospitalization,” spokesperson Kelly Malcom told the outlet.
To meet the criteria for monoclonal antibody treatment, “patients must have a positive COVID-19 test, be within a 7-10 day window of symptom onset, and be considered high-risk for severe disease,” the Detroit Free Press reports.
According to the outlet, “high-risk” individuals include those who are:
- 65 or older
- overweight or obese
- pregnant
- diabetic or with chronic kidney disease
- taking immunosuppressants or who has an immunosuppressive disease
- diagnosed with cardiovascular disease or high blood pressure
- diagnosed with chronic lung diseases such as COPD, asthma or cystic fibrosis
- diagnosed with sickle cell disease
- diagnosed with a neurodevelopmental disorder such as cerebral palsy or other conditions
- dependent on medical devices such as tracheostomy, gastrostomy or positive pressure ventilation.
- infants younger than age 1

This photo shows a hospital bed in one of the temporary rooms at the TCF Center, Monday, April 6, 2020, in Detroit. The city’s convention center was converted to accommodate an overflow of patients with the coronavirus. The U.S. Army Corps of Engineers began construction at the TCF Center to create a quarantined hospital setting with 1,000 beds as the pandemic spreads rapidly in the city. (AP Photo/Carlos Osorio)
The Omicron variant is a further potential strain on Michigan’s health system.
“All of the health systems … are at the breaking point,” Muma told the Detroit Free Press. “Every hospital I’ve talked to, every ER, is full of patients waiting for beds. There are no beds. People are sitting in the ER for days sometimes.”
“I don’t know how much we can take and you know, with omicron on the horizon, this could be devastating,” he added. “If we have yet another surge on in the middle of this surge, I don’t know what’s going to happen. I really don’t.”
In all likelihood, the variant will bring about increased illness rates and further squeeze monoclonal antibody supply, according to the Detroit Free Press:
That’s because lab studies suggest two of the three monoclonal antibody products on the market in the U.S. — those made by Regeneron and Eli Lilly — may not work well against the mutations found in the omicron variant, even though they were very effective in treating people who had the delta strain of the virus. More testing is under way.
The only monoclonal antibody therapy that has so far been shown to neutralize omicron in lab tests is a drug called sotrovimab, which is made by Vir Biotechnology and GlaxoSmithKline.
Muma is concerned that an increase in cases due to Omricon and the possibility of Eli Lilly’s monoclonal antibodies – “which is the one we have the most of, the one that’s in greatest production right now” – being ineffective against the strain, could “significantly limit the ability to administer these therapies.”
COMMENTS
Please let us know if you're having issues with commenting.