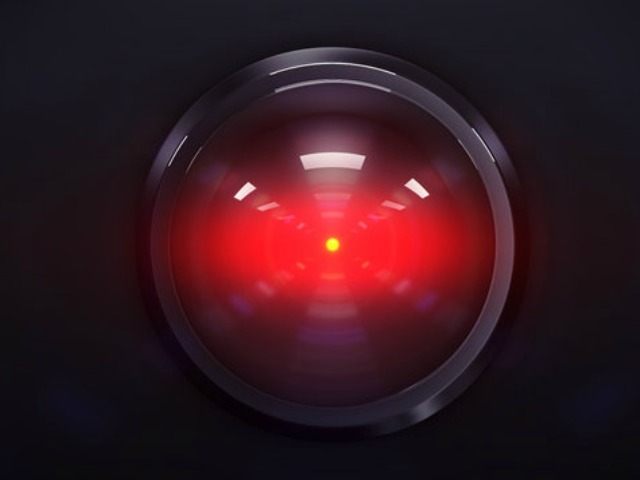
Cigna Healthcare, a major player in the health insurance industry, is now at the center of a federal class action lawsuit over claims that the company has been using AI algorithms to improperly deny customer claims. The lawsuit claims that Cigna’s system denied about 300,000 pre-approved claims, spending an average of 1.2 seconds to deny each claim.
Axios reports that major health insurance provider Cigna Healthcare is currently the target of a federal class action lawsuit. According to the lawsuit, the firm has been violating California law by utilizing AI algorithms to refuse payments to clients as part of a largely automated claims decision process.
The lawsuit, filed in the eastern district of California, claims that Cigna has been bypassing the requirement for medical professionals to conduct “thorough, fair, and objective” reviews of insurance claims. Instead, the company is accused of relying on its PxDx system, an abbreviation for procedure-to-diagnosis, to refuse claims en masse.
The lawsuit claims that over a two-month period in 2017, Cigna’s PxDx system was used to deny almost 300,000 pre-approved claims; the system allegedly took 1.2 seconds on average to deny each claim. It further alleges that a single Cigna medical director, Cheryl Dopke, rejected 60,000 claims over a single month.
The suit argues that Cigna has “wrongfully delegated their obligation to evaluate and investigate claims to the PxDx system,” and that the company has “fraudulently misled” its California customers “into believing their health plan would individually assess their claims.”
Interestingly, the lawsuit also reveals that of the claim denials that were appealed by Cigna customers, around 80 percent of the initial decisions were overturned. This statistic raises questions about the validity of the initial denials and the effectiveness of the PxDx system.
The California Department of Insurance is currently coordinating with other state regulators to investigate these claims.
“They’ve harnessed advancing technology not to improve people’s lives, but to summarily reject thousands of valid claims in the name of efficiency,” said Ryan Clarkson, managing partner of the public advocacy law firm handling the lawsuit.
Cigna has yet to comment on the lawsuit, but in the past, the company has dismissed criticisms of its PxDx system as “biased” and “incomplete.” As the case unfolds, it promises to be a landmark in the ongoing debate about the role of AI in healthcare and the balance between efficiency and fairness in the claims process.
Read more at Axios here.
Lucas Nolan is a reporter for Breitbart News covering issues of free speech and online censorship. Follow him on Twitter @LucasNolan

COMMENTS
Please let us know if you're having issues with commenting.